Pediatric cancer recurrence prediction has taken a significant leap forward with the advent of advanced artificial intelligence (AI) methodologies. Recent studies indicate that AI tools, particularly those trained on temporal data from brain scans, provide far more precise estimates of relapse risks compared to traditional techniques. This innovation is especially crucial for conditions such as gliomas, which are common pediatric brain tumors that, while often amenable to surgery, can pose a high risk of devastating relapse. By utilizing brain tumor imaging technology, researchers are able to glean insights that may lead to tailored follow-up care, alleviating the stress for both children and their families during their recovery journey. As we delve deeper into the intricacies of predicting cancer relapse with AI, it becomes evident that our approach to pediatric oncology is evolving dynamically, offering hope for improved patient outcomes and refined treatment pathways.
The realm of predicting pediatric cancer recurrence is witnessing transformative advancements thanks to innovative AI approaches. By leveraging techniques that assess changes in imaging data over time, researchers are better equipped to foresee potential tumor relapses in children diagnosed with brain cancers, such as gliomas. This enhanced ability to forecast relapse not only facilitates more effective monitoring but also paves the way for earlier intervention strategies. Employing advanced brain tumor imaging technologies, the medical community is on the cusp of redefining care standards in pediatric oncology. Through continuous exploration of temporal learning in medicine, we are uncovering essential patterns that can guide clinicians in their efforts to combat cancer recurrence.
The Role of AI in Pediatric Oncology
Artificial Intelligence (AI) is revolutionizing the landscape of pediatric oncology by enhancing predictive capabilities and personalizing treatment plans. In recent studies, AI has shown remarkable promise in analyzing vast amounts of medical imaging data, specifically the scans of patients with brain tumors like gliomas. These groundbreaking advancements are particularly crucial because they facilitate swift, accurate diagnosis and treatment strategies, ultimately improving outcomes for young patients. With algorithms tailored to recognize intricate patterns in imaging data, AI empowers oncologists to make informed decisions that can significantly affect a child’s prognosis.
Additionally, AI’s integration into pediatric oncology is not just limited to diagnostics. Ongoing research focuses on its potential in predicting treatment responses and assessing long-term outcomes. This expansive application aims to refine the precision of therapeutic interventions, as each patient’s tumor and response can differ vastly. By employing AI in various cinematic scenarios, the field is moving toward a future where treatment is tailored to individual needs, potentially minimizing side effects and maximizing survival rates.
Pediatric Cancer Recurrence Prediction with Advanced Techniques
Predicting the recurrence of pediatric cancers, especially gliomas, has traditionally been a challenging endeavor. However, the use of advanced AI techniques, such as temporal learning, has emerged as a groundbreaking approach to enhancing prediction accuracy. By analyzing multiple brain scans taken over time, researchers have developed models that assess the progression of tumors with a focus on identifying subtle changes that might signal a relapse. This increases the likelihood of detecting recurrence much earlier compared to conventional methods, significantly improving the chances for timely intervention.
The findings from recent studies indicate that AI techniques can predict the recurrence of both low- and high-grade gliomas with impressive accuracy rates ranging from 75% to 89%. Such substantial improvement over previous prediction models, which hovered around a mere 50%, highlights the transformative potential of incorporating AI technology in long-term patient monitoring. This shift could mean fewer unnecessary MRI scans for low-risk patients, tailored treatment plans for high-risk individuals, and ultimately, enhanced quality of care for pediatric patients facing battles with cancer.
Innovative Brain Tumor Imaging Technology
Brain tumor imaging technology has advanced significantly, thanks in part to the integration of artificial intelligence. Traditionally, medical imaging relied on static snapshots of a patient’s condition, often leading to misinterpretations or missed opportunities for timely intervention. The development of dynamic imaging techniques, incorporating AI, allows for a comprehensive analysis of brain tumor progression over time, offering deeper insights into tumor behavior and response to treatment. Such advancements in imaging ensure that oncologists are equipped with detailed data necessary for making critical treatment decisions.
Moreover, by employing sophisticated imaging technologies in tandem with AI algorithms, healthcare providers can achieve a more nuanced understanding of tumor characteristics. These technologies can highlight variations in tumor perfusion or metabolism, which are crucial indicators of tumor activity and potential malignancy. As researchers continue to explore the synergies between imaging technology and AI, the prospect of achieving more accurate diagnoses and personalized treatment plans becomes increasingly attainable, marking a significant step forward in pediatric oncology.
Temporal Learning in Medicine: A Game Changer
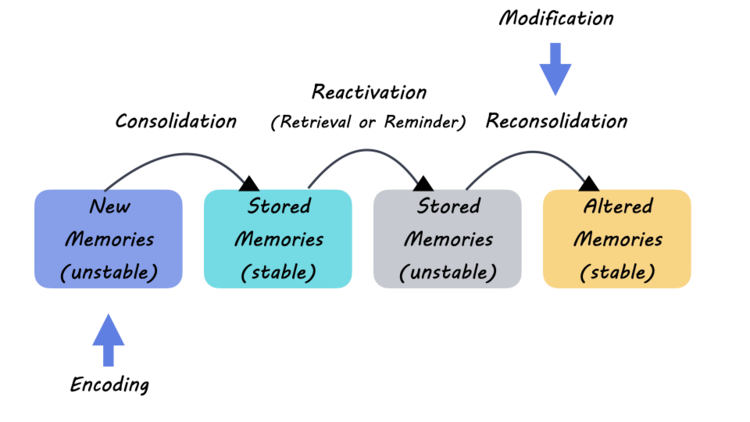
Temporal learning represents a revolutionary approach within the field of medical AI, particularly for managing pediatric cancers like gliomas. This technique involves training models to analyze sequences of imaging data collected over periods, rather than relying solely on isolated scans. By understanding the evolving nature of tumors through temporal analysis, AI tools can better predict which patients might face a recurrence and at what point post-treatment this might occur. This forward-thinking methodology not only heightens predictive accuracy but also opens pathways to potentially less invasive monitoring practices.
The implications of temporal learning extend beyond cancer recurrence predictions. By leveraging insights gathered from developing tumor characteristics, healthcare providers can customize monitoring schedules and treatment strategies for pediatric patients. For instance, a child identified as low-risk based on consistent imaging results may benefit from a less frequent MRI schedule, reducing the stress associated with rigorous testing. Conversely, identifying high-risk patients earlier ensures they can receive prompt, more aggressive treatments, drastically improving their chances of long-term survival.
Predicting Cancer Relapse with AI: The New Frontier
The ability to predict cancer relapse has long been a critical concern for oncologists, especially in the realm of pediatric care. Recent advancements utilizing AI technology are paving the way for more effective relapse predictions, fundamentally changing how medical professionals approach post-treatment monitoring. By analyzing diverse datasets—including longitudinal imaging and patient histories—AI can identify patterns and risk factors associated with cancer recurrence. This predictive capability not only streamlines patient care but also offers hope for improved outcomes for children battling cancer.
Moreover, the journey toward AI-driven relapse prediction is characterized by a commitment to ongoing research and validation. As the medical community eagerly anticipates the results from clinical trials leveraging these AI models, there is a promising potential for integrating AI insights into everyday clinical practice. The objective is to develop actionable guidelines based on AI findings, thereby equipping oncologists with the tools necessary to enhance patient safety and treatment efficacy. As this frontier unfolds, it stands to transform the landscape of pediatric oncology and ultimately give families the hope they desperately seek.
Enhancing Care with AI-Driven Risk Predictions
With the introduction of AI-driven models for predicting pediatric cancer recurrence, healthcare professionals are on the brink of a significant overhaul in patient management strategies. The ability to generate accurate risk predictions not only informs follow-up protocols but also allows oncologists to devise targeted treatment plans aimed at minimizing recurrence rates. Such predictive insights can guide decisions about imaging frequency, enabling more tailored care that aligns with the individual patient’s risk profile.
Furthermore, the promise of AI extends beyond mere prediction; it encompasses the potential for transforming treatment regimens based on relapse likelihood. For patients identified as high-risk, proactive measures such as the initiation of adjuvant therapies could be implemented earlier, potentially staving off devastating relapses. This focus on early intervention underscores the urgent need for continued research in AI applications within pediatric oncology, reinforcing the notion that enhancing care with predictive insights can lead to life-changing results for young patients and their families.
The Future of Pediatric Oncology Research
As the field of pediatric oncology evolves, the integration of AI technologies represents a pivotal advancement that promises to redefine treatment methodologies and patient outcomes. Ongoing research dedicated to exploring the capabilities of AI, particularly in predicting cancer recurrence and monitoring treatment responses, indicates a bright future ahead. With collaborative efforts among leading institutions, researchers are hopeful that the insights gleaned from AI analyses will yield clinically relevant breakthroughs, fostering innovations that cater specifically to the unique needs of pediatric patients.
In addition to enhancing predictive accuracy, the trajectory of AI in pediatric oncology emphasizes the importance of cross-disciplinary collaboration. By pooling expertise from data science, oncology, and radiology, researchers can continue to refine AI algorithms, ensuring they are robust and applicable across various patient demographics and tumor types. This concerted effort aims not only to improve individual patient outcomes but also to establish AI as an integral component of standard oncology practice, paving the way for a future where every child’s battle with cancer is met with the best possible tools and strategies.
AI and Ethical Considerations in Pediatric Care
As we stand on the cusp of an AI revolution within pediatric oncology, ethical considerations surrounding its use must also be taken into account. With advanced predictive algorithms capable of determining risk factors and treatment responses, it is essential to establish guidelines that prioritize patient consent, data privacy, and the equitable use of AI in healthcare settings. Striking a balance between innovation and ethical responsibility ensures that the benefits of AI technology are accessible to all pediatric patients, regardless of their background or healthcare resources.
Moreover, ensuring transparency in the development and implementation of AI systems within clinical environments is vital for building trust among patients, families, and healthcare providers. Clear communication about the capabilities and limitations of AI tools in predicting cancer relapse or guiding treatment plans is necessary to foster an informed approach to pediatric care. By committing to ethical practices, the pediatric oncology community can ensure that AI serves as a force for good, enhancing the quality of care while safeguarding the rights and dignity of vulnerable patient populations.
Clinical Trials: The Path to Improved Pediatric Cancer Care
As researchers continue to validate AI-driven predictions through clinical trials, the implications for pediatric cancer care are profound. The transition from theoretical models to real-world applications hinges on the successful outcome of these trials, aiming to refine techniques for predicting cancer recurrence and enhancing monitoring protocols. The anticipated results are expected to provide the groundwork for implementing AI technologies in clinical practice, thereby revolutionizing the follow-up process for pediatric patients with a history of gliomas.
Importantly, clinical trials not only test the efficacy of AI tools but also address patient outcomes holistically. By incorporating diverse populations and varying treatment histories, these trials aim to ensure that findings are representative and applicable to the broader pediatric oncology community. As we look forward to the outcomes of these studies, there is an optimistic outlook on the potential for AI to drive significant advancements, potentially leading to more effective and compassionate care for children battling cancer.
Frequently Asked Questions
What is pediatric cancer recurrence prediction and how is AI involved?
Pediatric cancer recurrence prediction involves assessing the likelihood of cancer returning in children after initial treatment. Recent advancements in AI are significantly improving this process. By employing machine learning techniques, such as temporal learning, AI can analyze brain scans over time to detect patterns indicative of cancer relapse, particularly in pediatric gliomas. This technology promises more accurate predictions compared to traditional single-scan methods.
How does AI enhance glioma relapse prediction in pediatric patients?
AI enhances glioma relapse prediction by analyzing multiple brain scans taken over different time periods. This approach, known as temporal learning, allows the AI model to recognize subtle changes in the scans that might indicate a risk of relapse. Research has shown that using this method can improve prediction accuracy to 75-89%, compared to the approximate 50% accuracy found with traditional imaging techniques.
What role does brain tumor imaging technology play in predicting pediatric cancer recurrence?
Brain tumor imaging technology is crucial in predicting pediatric cancer recurrence as it provides the visual data necessary for analysis. Through advanced imaging techniques like MRI, combined with AI algorithms, clinicians can track changes in a child’s brain tumor over time. This helps in identifying which patients are at higher risk of recurrence, ultimately guiding more personalized treatment plans.
What is temporal learning in medicine and its significance in pediatric cancer recurrence prediction?
Temporal learning in medicine refers to a method where AI systems analyze sequences of medical images over time to identify trends and changes. In pediatric cancer recurrence prediction, this technique allows for a comprehensive understanding of tumor progression, leading to more accurate forecasting of relapses. By integrating temporal learning, researchers have achieved significant improvements in prediction accuracy for conditions like pediatric gliomas.
Can AI effectively predict cancer relapse with AI in pediatric oncology?
Yes, AI can effectively predict cancer relapse in pediatric oncology. Studies have demonstrated that AI tools, when trained on serial imaging data, outperform traditional methods in predicting relapse risks. This is particularly evident in pediatric gliomas, where AI has shown an ability to detect early signs of recurrence, benefiting treatment decisions and potentially improving patient outcomes.
What are the benefits of using AI in predicting pediatric brain tumor recurrence?
The benefits of using AI in predicting pediatric brain tumor recurrence include increased accuracy in risk assessment, reduced unnecessary imaging frequency for low-risk patients, and earlier interventions for high-risk cases. AI models that utilize approaches like temporal learning can synthesize vast amounts of imaging data, thereby providing healthcare professionals with better tools to tailor treatments and follow-up strategies for young patients.
| Key Point | Details |
|---|---|
| AI Tool for Prediction | An AI tool outperforms traditional methods in predicting relapse risk for pediatric cancer patients. |
| Study Background | Conducted by researchers from Mass General Brigham, Boston Children’s Hospital, and others; results published in The New England Journal of Medicine AI. |
| Temporal Learning Technique | The AI model employs a technique called temporal learning to analyze multiple MR scans taken over time vs. a single scan. |
| Accuracy of Predictions | The temporal learning model predicts recurrence with 75-89% accuracy, significantly better than the 50% accuracy of single image analysis. |
| Future Implications | Potential to improve patient care by reducing unnecessary imaging or preemptively treating high-risk patients. |
Summary
Pediatric cancer recurrence prediction has seen a significant advancement with the introduction of an AI tool that improves accuracy in identifying relapse risks. This innovative approach leverages temporal learning from multiple brain scans, providing hope for better management and treatment of pediatric gliomas. As researchers work towards clinical trials, this technology may greatly enhance the quality of care for young cancer patients.