AI brain cancer predictions have emerged as a groundbreaking development in pediatric oncology, particularly in the realm of detecting and anticipating the recurrence of childhood brain tumors. A recent study from Mass General Brigham highlights how an AI tool significantly outperforms traditional methods by analyzing multiple brain scans over time, thereby offering a clearer picture of relapse risks associated with pediatric gliomas. This innovative approach to AI medical imaging focuses on temporal learning in AI, enhancing predictions through the synthesis of sequential MRI data. As pediatric gliomas often have varied prognoses, accurate prediction can pave the way for tailored interventions and optimized brain tumor treatments. Enhancing our understanding of cancer recurrence prediction not only benefits patients but also alleviates the emotional and physical toll on families navigating these challenging circumstances.
The advancements in artificial intelligence for predicting brain cancer recurrence represent a pivotal shift in pediatric cancer care. By employing sophisticated machine learning algorithms, researchers are now uncovering insights into the dynamics of brain tumors, specifically pediatric gliomas, which vary widely in their behavior and treatment responses. Through innovative applications of AI, especially temporal learning techniques, medical professionals can accurately track changes in brain scans over time, heightening the precision of cancer recurrence forecasts. This not only aligns with the goal of improving patient outcomes but also addresses the urgent need for effective strategies to manage follow-up procedures and treatment plans. As the landscape of pediatric oncology continues to evolve, the integration of AI into clinical practice holds immense promise for enhancing the quality of care and ensuring better prognoses for young patients.
The Role of AI in Pediatric Glioma Prediction
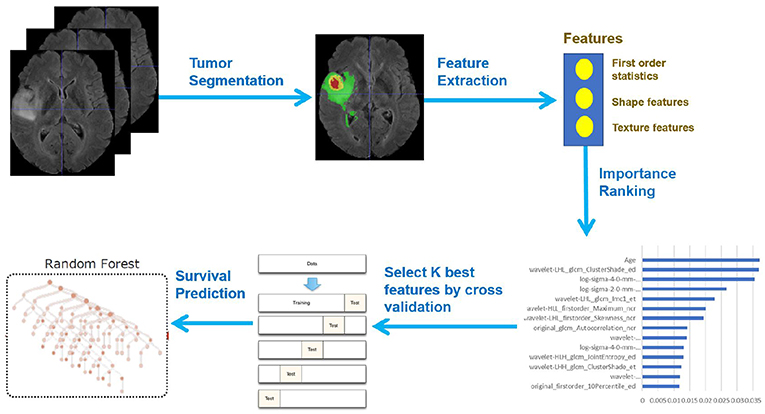
The incorporation of artificial intelligence (AI) into the realm of pediatric gliomas marks a significant advancement in how we predict and manage brain tumor recurrence. Traditionally, identifying children at risk for relapse relied heavily on a combination of experience and unreliable imaging techniques. However, AI is emerging as a powerhouse in this sector, transforming the accuracy of predictions significantly. Researchers have developed a sophisticated AI tool that utilizes temporal learning, allowing the model to analyze a series of MRI scans over time rather than a singular snapshot. This innovative methodology has shown a marked improvement in predicting which patients may experience a recurrence of their tumors, thus enhancing potential treatment pathways and outcomes for young patients.
Utilizing AI for cancer recurrence prediction offers not only higher accuracy but also alleviates the burden placed on families and children during the follow-up process. Frequent MRI screenings can be stressful and invasive; thus, being able to predict recurrence risks more accurately allows healthcare providers to streamline the monitoring process. For instance, less frequent imaging might be prioritized for low-risk patients while ensuring close monitoring of those identified as high risk. This predictive capability through AI is a promising leap forward, especially in managing pediatric gliomas, where timely interventions can greatly improve survival rates.
Understanding Temporal Learning in AI for Brain Cancer
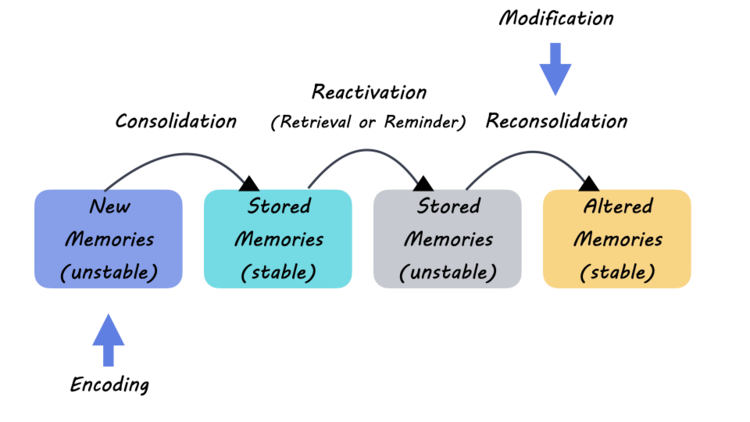
Temporal learning is an essential component of the recent advancements in AI applications for medical imaging, particularly in understanding the progression of brain cancers like pediatric gliomas. This innovative approach involves training AI models to analyze multiple images taken over time, capturing crucial subtle changes that individual scans might overlook. Unlike conventional methods that operate on single images, temporal learning allows for a more contextual understanding of tumor growth and behavior post-surgery. The integration of this technique enables researchers to predict the likelihood of cancer recurrence by establishing a timeline of the tumor’s characteristics as viewed across various MRI scans.
The Harvard study showcased the effectiveness of this technique, revealing that the AI model could predict glioma recurrence with an impressive accuracy of 75-89% by utilizing a series of scans rather than relying on isolated images. This development is groundbreaking as it exemplifies how AI can redefine predictive models in oncology. By accumulating data points and understanding changes over time, the AI not only becomes a predictive tool but also an agent in improving the quality of patient care, offering tailored recommendations for treatments based on individual pathology and risk factors.
Implications for Brain Tumor Treatments
The introduction of AI-driven predictions for pediatric gliomas has significant implications for treatment strategies and outcomes. By accurately predicting the likelihood of cancer recurrence, healthcare providers can adopt a more personalized approach to treatment planning. For instance, children identified as high-risk patients could receive pre-emptive targeted adjuvant therapies, which are designed to reduce the chances of tumor regrowth following initial treatments. Conversely, those deemed low-risk may benefit from reduced imaging frequency, alleviating the physical and emotional toll associated with rigorous monitoring.
In alignment with the advances in AI, new treatment protocols may also emerge as researchers delve deeper into understanding brain tumor behaviors and patient responses. As AI tools like the temporal learning model continue to evolve, their ability to synthesize vast quantities of imaging data could lead to more nuanced insights into effective treatment methodologies. By bridging the gap between AI medical imaging and clinical application, there is a favorable outlook for enhancing patient care in pediatric oncology, thus fostering higher survival rates and offering hope to families affected by brain cancers.
Enhancing Patient Care with Advanced Imaging Techniques
The advancement of AI in predicting brain cancer recurrence is not only revolutionizing the clinical approach but also enhancing overall patient care for those affected by gliomas. Advanced imaging techniques that leverage AI capabilities enable medical professionals to derive more meaningful insights from MRI scans. With tools that analyze multiple imaging data points over time, physicians are better equipped to make informed decisions regarding treatment protocols and follow-up care. This ensures that the management of pediatric gliomas is not merely reactive, but rather proactive, tailored to the specific needs of each patient.
Furthermore, the adoption of these cutting-edge imaging techniques can lead to a significant reduction in unnecessary interventions. By streamlining the follow-up protocols based on accurate risk assessments, children can experience less anxiety and disruption in their lives post-treatment. The shift towards a more data-driven, patient-centric care model reflects the broader trend of integrating technology into healthcare, aiming to refine treatment outcomes and improve the quality of life for young patients facing the challenges of brain tumors.
Future Directions in AI and Pediatric Oncology
The ongoing research into AI applications for predicting brain cancer recurrence in pediatric patients is paving the way for promising future directions in oncology. With proven results from studies exemplifying the capabilities of temporal learning, researchers are gearing up for clinical trials aimed at validating these AI-informed risk predictions in diverse healthcare settings. These trials will be crucial for determining the efficacy of incorporating AI tools into routine clinical practice and enhancing standard treatment protocols for pediatric gliomas.
Additionally, as more insights are gathered from the application of AI in medical imaging, there is potential for broader integration into various oncology specialties. As AI continues to develop and improve, it may also contribute to more comprehensive cancer recurrence prediction models across different types of tumors, not just pediatric gliomas. This expanding role of AI signals a future where data-driven methodologies might become the norm, giving healthcare professionals the tools they need to make informed, personalized decisions that could transform cancer care on a larger scale.
Challenges in Implementing AI in Clinical Settings
Despite the promising advancements brought by AI in predicting cancer recurrence, several challenges remain in implementing these technologies in clinical settings. One major concern is the validation of AI models across different populations and clinical environments. The accuracy demonstrated by studies, while impressive, needs to be consistently replicated in wider and more diverse cohorts to ensure the generalizability of the findings. Additionally, integrating these AI tools into existing healthcare systems requires not only technological upgrades but also staff training to effectively utilize AI insights for patient care.
Furthermore, there are ethical considerations surrounding the use of AI, particularly regarding data privacy, informed consent, and the potential implications of relying heavily on technology for critical healthcare decisions. As AI in medical imaging continues to evolve, it will be paramount for researchers and clinicians to address these challenges by fostering collaboration among stakeholders, including patients, healthcare providers, and technology developers, to establish guidelines that ensure safe and effective AI implementation.
The Significance of Early Detection in Pediatric Brain Tumors
Early detection of pediatric brain tumors such as gliomas is critical for improving patient outcomes. When identified promptly, treatment options can be implemented more swiftly, which often correlates with higher survival rates. The ability to predict recurrence effectively using AI tools not only contributes to better initial management but also empowers healthcare providers to monitor patients more strategically over time. By recognizing subtle changes captured in multiple MRI scans, clinicians can intervene earlier, potentially preventing severe complications that may arise from late-stage tumor recurrence.
This proactive posture in treating pediatric gliomas underscores the vital importance of continuous innovation in cancer care. As AI models refine their predictive capacities, the hope is that practitioners can integrate these insights into everyday clinical practice, ensuring that children receive the timely care they need. The overarching goal remains clear: to harness the power of technology to save lives and improve the future prognosis for children diagnosed with brain tumors, making early detection not just a goal, but a standard in pediatric oncology.
Parental Involvement in Treatment Decisions
The journey of managing a child’s brain cancer often involves crucial decisions that extend beyond the medical realm, necessitating parental involvement in treatment discussions and choices. With the introduction of AI tools that predict relapse risks, parents are called upon to understand these technologies and their implications for their child’s care. Effective communication between healthcare providers and families about the risks and benefits of AI-driven predictions can foster an environment of trust, allowing parents to take an active role in treatment decision-making.
Empowering parents with knowledge regarding AI medical imaging results can also help alleviate some of the fear and uncertainty that often accompany cancer diagnoses. By providing clear explanations and educational resources, healthcare professionals can help families comprehend how AI models function and their potential impacts on treatment pathways. As a result, parents may feel more confident in participating in discussions about the frequency of imaging and possible interventions, ensuring that care decisions align with the family’s values and preferences while optimizing outcomes for their child.
Advancements in Research Collaboration for Optimized Care
The collaborative nature of the research efforts highlighted in the study signifies a remarkable shift towards optimized care in pediatric oncology. By pooling resources and expertise from various institutions, researchers were able to analyze nearly 4,000 MRI scans from a substantial cohort of pediatric patients, enhancing both the volume and quality of data available for AI training. This collective approach not only accelerates research progress but also fosters a multidisciplinary environment where insights from different fields converge, creating more robust predictive models for brain cancer recurrence.
Moreover, such collaborations can lay the groundwork for future innovations that aim to tackle some of the pressing challenges in brain tumor treatment. By working together, healthcare facilities can share best practices and findings, ultimately leading to the development of standardized protocols that can be implemented across different contexts. As the landscape of pediatric oncology evolves with the integration of AI, the unified efforts of researchers and clinicians will be critical in driving advancements that benefit children facing the reality of brain tumors.
Frequently Asked Questions
How does AI brain cancer prediction improve the management of pediatric gliomas?
AI brain cancer predictions enhance the management of pediatric gliomas by utilizing advanced algorithms to analyze multiple MRI scans over time. This temporal learning approach increases the accuracy of predicting cancer recurrence, enabling healthcare providers to identify at-risk patients earlier and tailor follow-up treatments accordingly.
What role does temporal learning in AI play in cancer recurrence prediction for pediatric gliomas?
Temporal learning in AI allows predictive models to analyze sequential MRI scans taken over time, which helps identify subtle changes that may indicate cancer recurrence. This method significantly improves cancer recurrence prediction accuracy compared to traditional single-scan analyses.
Can AI medical imaging reduce the frequency of MRI scans in children with brain tumors?
Yes, AI medical imaging can potentially reduce the frequency of MRI scans for children with brain tumors by accurately predicting the risk of recurrence. For low-risk patients, AI-informed decisions may allow less frequent monitoring, alleviating stress on the child and family.
What is the impact of AI on brain tumor treatments for pediatric glioma patients?
AI enhances brain tumor treatments for pediatric glioma patients by providing precise predictions regarding recurrence risks. This insight enables clinicians to customize treatment plans, potentially employing targeted therapies for high-risk patients while sparing low-risk patients from aggressive follow-up measures.
How does AI improve the accuracy of cancer recurrence prediction in pediatric patients?
AI improves the accuracy of cancer recurrence prediction in pediatric patients by leveraging large datasets of sequential MRI scans. The AI algorithms utilize temporal learning to detect patterns over time, leading to a more informed assessment of individual patient risks compared to traditional methods.
What potential does AI hold for future research in pediatric cancer care?
AI holds significant potential for future research in pediatric cancer care, particularly in the prediction of recurrence and personalization of treatment strategies. By integrating AI brain cancer predictions into clinical practice, researchers hope to enhance patient outcomes and reduce the burden of unnecessary imaging.
| Key Points |
|---|
| AI tool predicts relapse risk in pediatric brain cancer patients more accurately than traditional methods, particularly for gliomas. |
| The study involved nearly 4,000 MRI scans from 715 patients, published in The New England Journal of Medicine AI. |
| Temporal learning technique was used, training the model on multiple scans over time rather than individual scans. |
| The AI model achieved a prediction accuracy of 75-89%, much higher than the 50% accuracy of single-image predictions. |
| Further validation and clinical trials are necessary before practical application in patient care can commence. |
| The goal is to optimize treatment through AI by reducing unnecessary imaging and targeting high-risk patients with therapy. |
Summary
AI brain cancer predictions have shown significant promise in the early identification of relapse risk among pediatric patients. Through advanced methodologies such as temporal learning, researchers are striving to revolutionize the way brain cancer is monitored and treated, offering hope for more tailored and less burdensome healthcare interventions.