Pediatric cancer recurrence prediction is at the forefront of a groundbreaking new study that leverages AI technology to enhance outcomes for children facing gliomas and other brain tumors. Traditional methods of assessing relapse risk have proven inadequate, demanding frequent and sometimes anxiety-inducing imaging procedures for young patients and their families. However, with AI tools designed for pediatric oncology, researchers have developed advanced predictive models that significantly outperform these outdated techniques. By employing innovative approaches, such as temporal learning in medicine, these predictive models analyze data over time rather than relying solely on individual scans, offering hope for more accurate and timely interventions. As the field of pediatric cancer care continues to evolve, the integration of glioma predictive modeling and pediatric cancer AI tools represents a pivotal step towards improving treatment and forecasting risks associated with brain tumor management.
In the realm of childhood cancer, predicting the likelihood of relapse is becoming increasingly sophisticated. Utilizing state-of-the-art technology, experts are employing advanced artificial intelligence approaches to improve the assessment of recurrence risks in young patients diagnosed with tumors like gliomas. Traditional imaging practices often fall short in delivering precise insights, prompting a shift towards innovative brain tumor risk assessment methods. By analyzing sequences of imaging data over time—known as temporal modeling—medical professionals can gain deeper insights, leading to better-informed decisions about treatment pathways for children. This evolution in the healthcare landscape signifies a crucial step forward in ensuring that pediatric cancer survivors receive the most tailored and effective care possible.
The Importance of Early Detection in Pediatric Cancer
Early detection plays a critical role in improving outcomes for pediatric cancer patients. The earlier a cancer is identified, the more treatment options are available, and the better the chances of recovery. Traditional methods have often relied heavily on scheduled imaging and assessments to monitor at-risk children, which can be stressful and lead to over-treatment or under-treatment. With advancements like AI in pediatric oncology, healthcare providers can utilize more refined tools to identify cases needing immediate attention, thereby alleviating some stress from families and optimizing patient care.
The integration of AI tools into pediatric oncology is revolutionizing the approach to disease management, shifting the paradigm from reactive to proactive treatment strategies. AI-driven insights can help clinicians predict potential complications, monitor disease progression, and tailor interventions based on individual patient data. By assessing multiple parameters, including those gathered through MRI scans and medical histories, healthcare teams can form a comprehensive view of a patient’s health, resulting in better management of treatment plans and a reduction in anxiety for families and children undergoing these processes.
Advancements in AI Tools for Cancer Risk Assessment
Recent studies have highlighted significant advancements in AI tools designed for cancer risk assessment, specifically in the realm of pediatric gliomas. These AI technologies leverage extensive data sets and advanced algorithms to analyze patterns and predict outcomes. For instance, the temporal learning method utilized in recent research allows AI models to evaluate multiple brain scans over time, rather than just isolated images. This presents a tremendous opportunity for clinicians to understand how tumors evolve, and which patients may be at risk for recurrence, thereby enhancing the personalization of treatment strategies.
By adopting these innovative AI tools, healthcare providers are better equipped to deliver accurate prognosis and timely interventions. The ability of AI to analyze comprehensive imaging data and recognize subtle changes that may indicate a potential relapse marks a substantial improvement over traditional methods, which often rely on single scans with limited contextual insight. As a result, pediatric cancer AI tools are not only enhancing predictive modeling but are also fostering a deeper understanding of various cancer types, ultimately leading to improved patient outcomes.
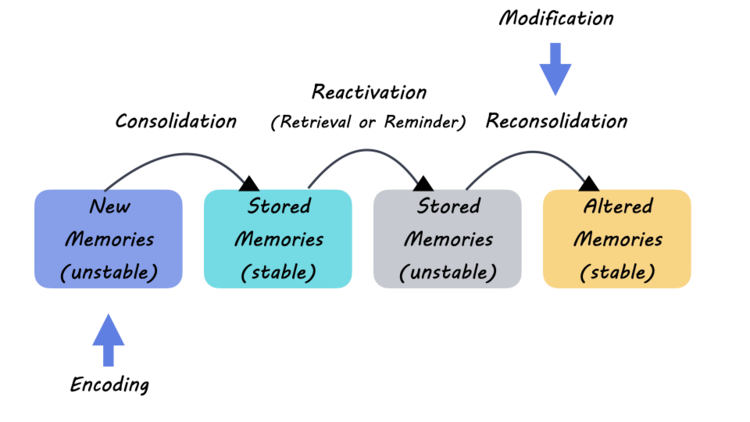
The Role of Temporal Learning in Predictive Modeling
Temporal learning represents a groundbreaking shift in the field of predictive modeling, especially within pediatric oncology. This technique allows AI systems to draw connections between sequential data points, such as periodic MRI scans of a patient’s brain. By analyzing the progression of the tumor over time, rather than relying on static images, AI can detect changes that might not be visible in single assessments. This advance is crucial for accurately predicting pediatric cancer recurrence, as it brings a level of insight that enhances clinical decision-making.
Implementing temporal learning in medical imaging signifies a promising future where AI can provide more nuanced predictions based on a timeline of patient data. This approach is particularly beneficial in dealing with gliomas, where treatment pathways can vary widely among patients. With the ability to predict recurrence risk more accurately, healthcare teams can devise tailored surveillance plans, ensuring that children at higher risk receive appropriate monitoring and treatment interventions, thereby improving overall outcomes.
Predicting Pediatric Cancer Recurrence: The New AI Method
The challenge of predicting pediatric cancer recurrence has been a significant concern for clinicians and families. Traditional assessment mechanisms often lead to emotional and financial burdens due to frequent imaging and the stress associated with uncertainty in prognosis. However, the newly developed AI method has shown promise in predicting recurrence rates of gliomas with remarkable accuracy, ranging from 75% to 89%. This leap in predictive capability can potentially transform the management of pediatric brain tumors and reassure families about their child’s health.
As researchers continue to validate and optimize this AI model, the hope is to streamline the follow-up processes for younger patients, reducing unnecessary imaging while maintaining precision in risk assessment. The strategic application of AI for predicting pediatric cancer recurrence not only enhances the accuracy of clinical predictions but also alleviates some of the anxieties faced by families. Understanding the likelihood of recurrence will empower healthcare teams to customize treatment plans effectively, focusing on early intervention for those at risk.
Collaboration in Pediatric Cancer Research
Collaboration across institutions is key to advancing pediatric cancer research and treatment options. Recent studies undertaken by Mass General Brigham, Boston Children’s Hospital, and Dana-Farber illustrate the synergy that comes from combining resources and expertise. This comprehensive approach enables the collection of extensive datasets, crucial for training AI models that identify patterns related to gliomas and other pediatric cancers. Collaborative research efforts are paving the way for innovative tools that enhance the precision of patient assessments.
Involving multiple stakeholders allows for shared insights and breakthroughs in predictive modeling and the development of new AI-driven methodologies. This reinforces the notion that multidisciplinary teamwork is essential in overcoming the complexities of pediatric oncology and ensuring that children receive the best possible care. By leveraging collective knowledge and diverse resources, researchers can foster innovation that significantly improves the outlook for pediatric cancer patients.
AI’s Capacity to Change Treatment Protocols in Pediatric Oncology
The ongoing integration of AI technologies is set to revolutionize treatment protocols in pediatric oncology. With the ability to enhance predictive accuracy, these tools provide clinicians with data-driven insights that can lead to more personalized treatment approaches. For instance, understanding recurrence risks through AI-enabled assessments allows healthcare providers to optimize follow-up care and adjust treatment plans proactively rather than reactively. This shift could greatly improve patient management and outcomes.
Moreover, the incorporation of AI can aid in identifying patients who require intensive monitoring and those who can safely reduce the frequency of imaging. As clinicians begin to tailor their approaches based on AI predictions, not only does this streamline resource allocation, but it also reduces the emotional impact of prolonged uncertainty on the families. By adapting treatment protocols informed by cutting-edge tools, health professionals can ensure a more focused and effective care experience for pediatric cancer patients.
The Future of Pediatric Cancer AI Tools
The future of pediatric cancer care looks promising with the continued development of AI tools designed specifically for oncology. As researchers refine these technologies, the potential applications are vast, ranging from improved predictive modeling of tumor behavior to individualized treatment protocols. Continuous advancements in AI methodologies, such as the implementation of temporal learning, suggest that we might soon reach a point where prediction accuracy in oncology becomes standard practice, markedly improving patient outcomes.
Furthermore, as AI tools become more widespread in pediatric oncology, they will not only assist clinicians in making informed decisions but also empower families with the knowledge needed to navigate their child’s treatment journey effectively. As these AI technologies advance and gain acceptance, they will herald a new era of precision medicine in pediatric cancer care, ultimately improving survival rates and enhancing the quality of life for young patients.
Impact of AI on Patient and Family Experiences
The introduction of AI tools in pediatric oncology not only benefits clinical outcomes but also significantly enhances the experiences of patients and their families. The stress associated with frequent MRI scans and the uncertainty of a child’s prognosis can take a toll on families. However, with AI’s ability to predict recurrence risks and streamline monitoring processes, families are likely to experience a reduction in anxiety related to prolonged uncertainty about their child’s health.
Empowering families with clear, data-driven insights into their child’s condition allows them to engage more actively in treatment decisions. This shift creates an environment of collaboration between families and healthcare providers, fostering an approach that softens the burden of illness. The optimistic outlook supported by AI tools provides hope and reassurance to families, motivating them to navigate the challenges of pediatric cancer with confidence.
The Need for Continued Research in Pediatric Cancer
While significant strides have been made in using AI to predict pediatric cancer recurrence, continued research remains vital. Each new study not only builds on existing knowledge but also brings forth new questions and challenges that need to be addressed. As technology evolves, it is crucial for researchers to remain dedicated to understanding the complexities of pediatric cancers and the unique biological behavior of tumors amongst young patients.
Innovative research pathways, including collaboration with institutions and the integration of diverse perspectives and expertise, will drive forward the momentum required in this field. Ongoing trials and studies will allow researchers to test the applicability of new methodologies, ensuring that the latest advancements in AI and predictive modeling are effectively translated into clinical practice. This commitment to research is what will ultimately enhance patient care, improve treatment outcomes, and provide comprehensive strategies for managing pediatric cancers.
Frequently Asked Questions
What role does AI in pediatric oncology play in predicting cancer recurrence?
AI in pediatric oncology has shown significant potential in predicting the recurrence of pediatric cancers. By analyzing multiple brain scans over time, AI tools can outperform traditional methods, providing doctors with better insights into which patients are at high risk for relapse, particularly in conditions like gliomas.
How effective is glioma predictive modeling in assessing relapse risk in pediatric patients?
Glioma predictive modeling using advanced AI techniques, such as temporal learning, has demonstrated accuracies between 75% and 89% in predicting cancer recurrence, a notable improvement over the traditional methods that offered around 50% accuracy. This modeling helps identify patients who may require closer monitoring or preventive treatments.
What advancements have been made in pediatric cancer AI tools for recurrence prediction?
Recent advancements in pediatric cancer AI tools include the use of temporal learning to analyze sequential MRI scans. This innovation enables the AI to detect subtle changes that indicate the likelihood of recurrence, facilitating more personalized treatment strategies and reducing the strain of frequent imaging on young patients.
How does brain tumor risk assessment utilize AI technologies in pediatric oncology?
Brain tumor risk assessment in pediatric oncology is enhanced by AI technologies that analyze large datasets of imaging scans. AI models can gather insights from historical patient data and trends, leading to more accurate predictions for potential tumor recurrence and optimizing follow-up care.
What is the significance of temporal learning in predicting pediatric cancer recurrence?
Temporal learning is crucial in predicting pediatric cancer recurrence as it allows AI models to analyze sequences of brain scans over time, capturing subtle trends and changes linked to malignancies. This method significantly improves prediction accuracy and guides treatment decisions in pediatric oncology.
Can AI help reduce the frequency of imaging for low-risk pediatric cancer patients?
Yes, AI has the potential to reduce the frequency of follow-up imaging for low-risk pediatric cancer patients. By employing AI-driven predictions, clinicians can determine which patients require less intensive monitoring, alleviating both the burden on the child and the healthcare system.
What are the future prospects for AI in pediatric cancer recurrence prediction?
Future prospects for AI in pediatric cancer recurrence prediction include ongoing clinical trials to validate AI tools across diverse settings. Researchers aim to refine these technologies for broader clinical application, which could lead to more effective and tailored treatments for pediatric oncology patients.
| Key Points | Details |
|---|---|
| AI Tool Development | An AI tool developed to analyze brain scans shows better predictive capabilities for pediatric cancer relapse than traditional methods. |
| Significant Findings | The AI tool predicts recurrence of pediatric gliomas with 75% to 89% accuracy, compared to 50% accuracy from individual scan methods. |
| Research Collaboration | The study was a collaborative effort between Mass General Brigham, Boston Children’s Hospital, and the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. |
| Temporal Learning Use | This technique trains the AI using multiple scans over time, allowing it to recognize subtle changes in patient conditions. |
| Next Steps | Further validation and clinical trials are needed to confirm efficacy and improve patient care through targeted treatment. |
Summary
Pediatric Cancer Recurrence Prediction has seen significant advancements with the introduction of AI tools capable of analyzing multiple brain scans. This innovative approach not only enhances the accuracy of predicting relapse risks but also aims to alleviate the burdens faced by families during the follow-up process. As the research progresses towards clinical application, the potential benefits for pediatric oncology patients are promising, paving the way for tailored treatments and improved care strategies.