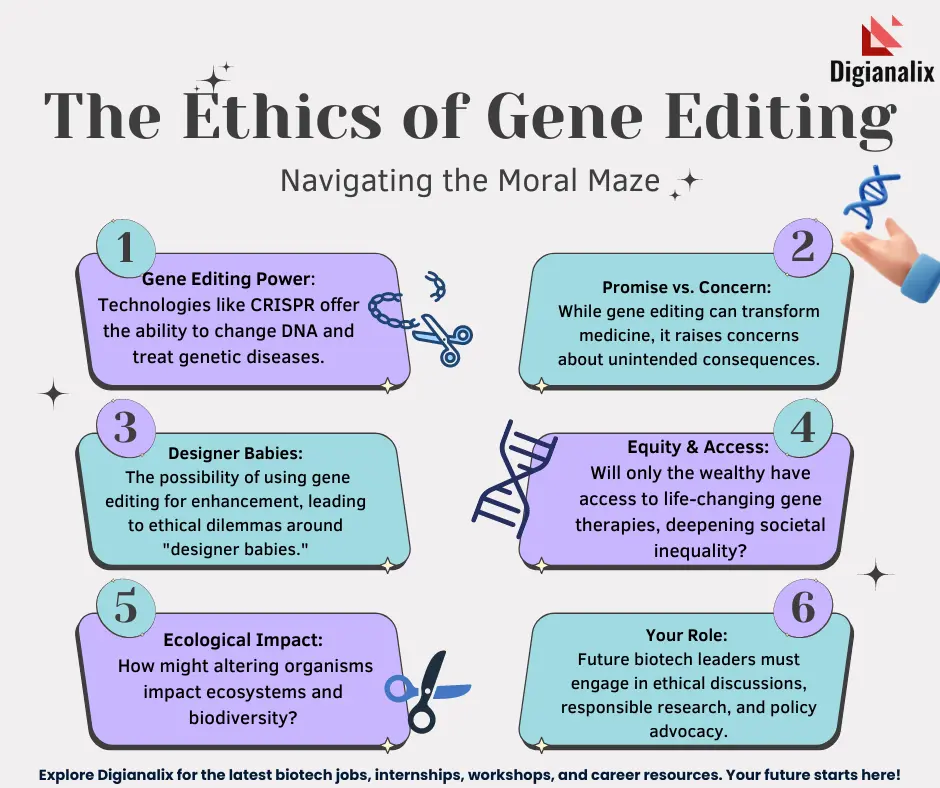
Gene editing ethics is an increasingly vital topic as advancements in CRISPR technology revolutionize medicine and raise crucial questions about our ability to alter human genetics. This innovative approach has opened up possibilities for groundbreaking treatments, such as a potential sickle cell anemia cure, but it brings with it profound ethical implications of gene editing that society must grapple with. As scientists manipulate genes through gene therapy, the conversation shifts to the broader health equity issues surrounding access to these treatments—who benefits and who gets left behind? In discussions led by experts, the promise of curing debilitating diseases stands against the backdrop of moral dilemmas about what it means to be human. These competing narratives necessitate a nuanced analysis of how far we should go in our pursuit of genetic modification and the responsibility that comes with such power.
The ethics of genetic modification encompasses a spectrum of considerations as we venture into the future of medical science and human enhancement. With the advent of genetic engineering techniques, notably CRISPR, the potential to eradicate hereditary conditions and enhance human traits is rapidly becoming a reality. However, as we explore avenues such as gene therapy to combat ailments like sickle cell disease, we must also confront the societal ramifications of these innovations. Discussions surrounding the responsibility of genetic interventions often touch on themes of health equity and whether new technologies will equally serve diverse populations, or deepen existing disparities. As we navigate these complex issues, it is paramount that we balance the quest for scientific progress with ethical prudence.
The Promise of CRISPR Technology in Medicine
CRISPR technology has revolutionized the field of genomics, enabling targeted gene editing with unprecedented precision. This innovation holds potential not only for curing genetic diseases like sickle cell anemia but also for enhancing our understanding of various biological processes. With its capability to modify somatic cells and embryonic germlines, CRISPR opens new avenues in gene therapy, representing a promising frontier in medical science that could eradicate certain genetic disorders from future generations.
Moreover, the application of CRISPR technology in medical treatments demonstrates significant promise for improving health outcomes. For instance, researchers have successfully used CRISPR to modify cells in patients suffering from sickle cell anemia, significantly reducing the disease’s debilitating effects. As clinical trials continue to validate these approaches, the prospect of widespread adoption of gene editing in therapeutic practices becomes increasingly feasible, showcasing how instrumental advancements in technology can lead to breakthroughs in health.
However, with great power comes great responsibility. As we venture deeper into utilizing CRISPR for practical applications, the necessity for stringent ethical oversight becomes evident, emphasizing the fine line between treatment and enhancement. Ensuring equitable access to such groundbreaking therapies is crucial to avoid widening the existing health equity gap. Thus, while CRISPR provides a beacon of hope for patients, it also beckons a thorough examination of its implementation in the medical field.
Balancing innovation with ethical considerations requires collaborative efforts among scientists, ethicists, and policymakers. Engaging in discussions about the implications of gene editing must include perspectives from diverse communities to ensure that advancements benefit all facets of society. As CRISPR technology continues to evolve, addressing potential inequalities and ethical concerns will be paramount in shaping a responsible future in medicine.
Ethical Implications of Gene Editing
The advent of gene editing technologies, particularly CRISPR, raises profound ethical questions about the nature of humanity and the essence of genetic diversity. The debate often centers on whether we have the right to alter the genetic makeup of individuals, especially when it comes to diseases that are not deemed life-threatening. This dilemma is exemplified by Baer’s questions regarding the ethics of editing genes for conditions compatible with life, such as Down syndrome, leading to contentious discussions on parental rights and societal values.
The ethical implications extend to issues of consent and the potential commodification of human life. Who can make decisions about genetic enhancements, and how do we ensure these choices consider the welfare of the individual, particularly when it involves unborn children? As seen in the discussion surrounding cases of genetic modification for traits like hearing, the power to choose attributes raises concerns about eugenics and what it means to accept human variation. These ethical quandaries necessitate comprehensive dialogues to navigate the complex landscape of gene editing thoughtfully.
Furthermore, the discussions inevitably touch upon health equity issues that intersect with technology. The exorbitant cost associated with advanced gene therapies, such as the $2.2 million price tag for curing sickle cell disease, brings to the forefront the disparity in access to such modalities. The question remains: who gets to benefit from these innovative treatments, and at what cost? The risks of deepening existing inequities are significant if access to life-saving therapies becomes a privilege rather than a right.
Addressing these ethical implications requires a holistic approach that incorporates diverse perspectives to shape policies and practices in gene editing. As we forge ahead, we must aim to create a framework that prioritizes health justice and inclusivity, ensuring that advancements in gene editing serve to uplift all communities rather than exacerbate existing disparities. The responsibility lies in undertaking ethics in tandem with innovation, fostering a future where technology enhances human experience without compromising our moral compass.
Lastly, oversight appears as a critical factor in regulating gene editing practices. Baer’s remarks on the potential for unregulated experimentation in countries lacking stringent laws raise urgent concerns about the international ramifications of gene editing. The prospect of genetic manipulation in military applications, as highlighted during the discussion, underscores the unforeseen consequences that could arise if such technologies fall outside ethical boundaries. Ensuring that the global community collectively addresses these concerns can help safeguard against misuse and promote responsible scientific exploration.
Health Equity and Gene Therapy Access
The issue of health equity is intrinsically linked to the advancements in gene therapy, as CRISPR technology continues to yield groundbreaking potential for treating genetic disorders. The ability to cure conditions like sickle cell anemia is a monumental achievement, but access to such innovative treatments remains a significant barrier for many underserved populations. The high costs associated with gene therapies emphasize the urgent need for systemic changes in healthcare to ensure equitable access to life-saving treatments.
Moreover, disparities in healthcare access often correlate with socioeconomic status, race, and geography, further complicating the landscape of gene therapy distribution. As discussions surrounding the implementation of CRISPR technology unfold, it is crucial to openly address how these disparities might be addressed. Initiatives must focus on creating pathways for reduced costs and increased accessibility, ensuring that all individuals, regardless of their background, have the opportunity to benefit from advancements in gene editing.
Simultaneously, addressing health equity issues necessitates a commitment to comprehensive public policy reforms that prioritize marginalized communities. By fostering partnerships between healthcare providers, policymakers, and patient advocacy groups, society can work to dismantle barriers that prevent equitable access to gene therapies. Engaging in collaborative efforts to address the underlying structural inequities in the healthcare system will be essential to harnessing the full potential of gene editing for all.
Ultimately, the combination of scientific advancement and equitable health policies can pave the way for a future where genetic disorders are treated effectively, and health equity becomes a reality rather than an aspiration. As stakeholders in healthcare continue to navigate the complexities of gene editing, prioritizing health equity will be paramount in achieving a just and inclusive framework that benefits everyone.
Future Prospects of Gene Editing Technology
The future of gene editing technology holds exciting possibilities that could transform medicine and the way we understand genetics. As CRISPR and other gene-editing tools become more sophisticated, researchers anticipate advancements that may not only cure genetic disorders but also enhance overall health and longevity. The prospect of eradicating diseases before birth or tailoring treatments to individual genetics represents a significant leap forward in personalized medicine.
However, alongside these advancements lies a need for cautious optimism. As science pushes boundaries, ethical considerations must evolve in tandem to address emerging dilemmas associated with gene editing. Factors such as environmental impacts, societal implications, and unforeseen genetic consequences must be thoroughly explored to ensure responsible innovation. The scientific community, in collaboration with ethicists and public stakeholders, must actively engage in dialogues that promote responsible practices and safeguarding against potential misuse.
For gene editing technology to reach its full potential, it will be crucial to foster a culture of transparency and inclusivity. By involving diverse voices in the conversation, we can strive to create a vision where gene editing serves the greater good, ensuring equitable access and addressing concerns about the moral implications of altering human genetics. By embracing a thoughtful approach to future advancements, we can lay the groundwork for a more equitable and ethically sound application of gene editing technology.
Ultimately, the responsibility for the future evolution of gene editing rests in our hands. As a society, we must aim to balance the promise of scientific innovation with an unwavering commitment to ethical consideration, ensuring that the technologies we develop benefit all and do not compromise the fundamental values that define human existence.
Frequently Asked Questions
What are the ethical implications of gene editing using CRISPR technology?
The ethical implications of gene editing with CRISPR technology are vast, encompassing concerns about the modification of human embryos, the potential for eugenics, and the long-term effects on genetic diversity. Critics argue that editing genes could lead to unforeseen consequences, impacting not just the individual but future generations. Additionally, the decision of which traits to modify raises moral dilemmas about parental rights and societal norms.
How does gene editing technology like CRISPR offer a cure for sickle cell anemia?
CRISPR technology allows for the precise editing of genes responsible for sickle cell anemia by targeting and correcting the specific mutations within the DNA. This gene therapy approach has shown promise in clinical trials, providing a potential permanent cure by enabling patients to produce healthy red blood cells. However, the associated ethical questions about access and equity in healthcare must also be considered.
What role does health equity play in discussions about gene therapy?
Health equity is a critical issue in gene therapy discussions, particularly regarding costly treatments like CRISPR-based cures. The high expenses associated with such therapies may limit access for underprivileged populations, leading to greater health disparities. As gene editing becomes more prevalent, it is essential to address these equity issues to ensure that advancements benefit all segments of society, rather than exacerbating existing inequalities.
Should gene editing be used to eliminate conditions like Down syndrome?
The question of whether gene editing should be employed to eliminate conditions such as Down syndrome raises significant ethical concerns. Proponents argue that it could prevent suffering, while opponents emphasize the value of diversity and the potential ‘slippery slope’ towards selecting traits. This debate questions the role of societal norms in determining which traits are considered undesirable and who gets to make those choices.
What are the risks involved in gene editing, particularly concerning unintended consequences?
Using gene editing technologies like CRISPR carries risks of unintended consequences. Modifying genes can lead to unexpected interactions and effects, potentially harming individuals in ways that are not initially apparent. For instance, altering a gene related to cholesterol has broader implications for overall health. Thus, thorough research and regulatory oversight are crucial to mitigate these risks before widespread application.
| Key Points | Details |
|---|---|
| CRISPR Technology | A gene-editing tool that allows for the modification of somatic and germline genes. |
| Ethical Concerns | Questions arise regarding the appropriateness of gene editing for conditions like Down syndrome. |
| Cost and Accessibility | High costs of treatments (e.g., $2.2 million for sickle cell) raise issues of equity. |
| Human Variation | Concerns about altering traits in children, particularly for those with disabilities. |
| Overreach and Oversight | Questions about the regulation of gene editing, especially in countries with less oversight. |
| Unintended Consequences | Editing genes can have complex and unforeseen effects on health and biology. |
Summary
Gene editing ethics is a critical topic that explores the moral implications of using technologies like CRISPR to modify human genes. As scientists gain the ability to alter DNA, fundamental questions about the impact on human identity and the consequences of such changes come to the fore. With powerful capabilities to cure diseases like sickle cell anemia, society must grapple with the ethical dilemmas regarding the value of human diversity and the potential repercussions of altering our genetic makeup.