Maternal mortality remains a pressing issue in the United States, where pregnancy-related deaths are alarmingly high compared to other high-income countries. Recent studies highlight the disturbing trend of rising maternal mortality rates, with large disparities evident based on race and geography. Over 80% of these deaths are preventable, underscoring the urgent need for improved maternal health strategies and postpartum care. The complexities contributing to this crisis range from inadequate healthcare access to systemic health disparities in pregnancy that disproportionately affect marginalized communities. Addressing maternal mortality is not merely a medical concern; it is a societal imperative that necessitates comprehensive reform in healthcare systems.
When discussing pregnancy-related fatalities, also referred to as maternal mortality, many factors come into play that highlights the need for urgent action. The alarming increase in these deaths—especially among racial minorities—exemplifies a significant public health challenge. Inequitable access to quality maternity care and inadequate postpartum support contribute to the high maternal mortality rates seen across the U.S. Furthermore, understanding the underlying health disparities in pregnancy can guide future interventions to prevent these tragic outcomes. Hence, it is critical to address the multifaceted nature of maternal health to ensure that all women receive the care they deserve throughout their pregnancy journey.
Rising Rates of Maternal Mortality in the U.S.
The United States continues to experience alarmingly high rates of maternal mortality, outpacing other high-income nations. This concerning trend highlights a critical healthcare crisis, where the majority of pregnancy-related deaths are deemed preventable. Recent research has shown that from 2018 to 2022, there has been a notable increase in maternal mortality rates, escalating from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. Such numbers are troubling, especially when we consider that a significant portion of these deaths could be avoided through better healthcare interventions, driving home the need for urgent action to improve maternal health outcomes across the country.
Moreover, the disparities observed in maternal mortality rates are stark and unsettling. For instance, American Indian and Alaska Native women suffer from mortality rates nearly four times higher than their white counterparts, underlining the systemic inequities present in maternal healthcare. This divergence in outcomes emphasizes the necessity for tailored healthcare solutions that address the unique challenges faced by different racial and ethnic groups. As we reflect on these findings, it becomes evident that a multifaceted approach – involving policy change, improved healthcare access, and enhanced postpartum care – is essential to truly tackle the rising maternal mortality rates in the U.S.
Addressing Health Disparities in Pregnancy Care
Health disparities in pregnancy are a persistent issue that continues to undermine maternal health in the United States. Factors such as socioeconomic status, access to healthcare, and systemic biases contribute to these disparities, leading to vastly different experiences and outcomes for pregnant individuals based on their race and ethnicity. The alarming statistics reveal that non-Hispanic Black women and American Indian women are disproportionately affected by high maternal mortality rates. Addressing these disparities calls for a concerted effort to reform policies and healthcare systems that currently fail to provide equitable care for all.
Targeted interventions, culturally competent care, and comprehensive support systems are vital components in overcoming these disparities. By assessing and revamping existing healthcare frameworks, states can better serve communities that are at greater risk. For instance, programs focused on community-based engagement and education can empower marginalized groups, ensuring they receive adequate prenatal monitoring and postpartum care. Ultimately, advancing maternal health means navigating the complexities of systemic inequality while simultaneously advocating for policies that foster access and equity across healthcare settings.
The Importance of Comprehensive Postpartum Care
Postpartum care, which encompasses a year following childbirth, is crucial for improving maternal health outcomes and reducing mortality rates. Despite the critical nature of this care phase, it is often overlooked in favor of immediate postpartum visits. The current healthcare framework frequently neglects the ongoing health challenges many women face after giving birth, which can lead to preventable late maternal deaths. This gap in comprehensive care underscores the need for healthcare systems to shift their focus from short-term to long-term wellness strategies, enhancing the continuity of care that women receive after childbirth.
Late maternal deaths, those occurring between 42 days and one year postpartum, account for nearly a third of all maternal deaths in the U.S. This statistic underscores the importance of integrated care that extends beyond the traditional six-week postpartum checkup. Initiatives that prioritize continuous monitoring and early intervention for chronic health issues, such as cardiovascular disease and hypertension, can significantly reduce these unforeseen fatalities. Strategies that foster stronger connections between patients and healthcare providers during the postpartum period can enhance support systems, ultimately contributing to better health outcomes for families and communities.
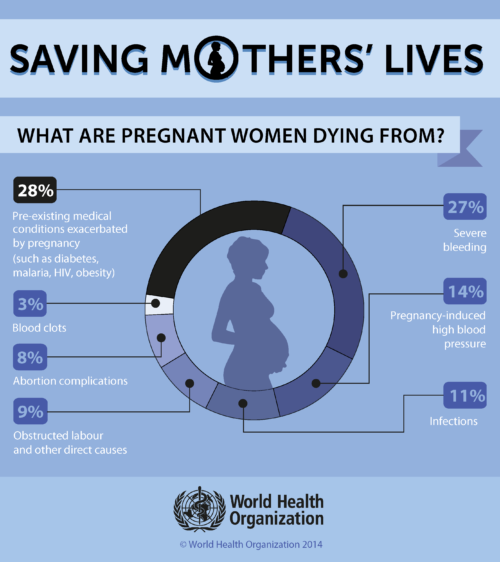
Understanding the Shift in Causes of Pregnancy-Related Deaths
Historically, pregnancy-related deaths were predominantly attributed to hemorrhage and infection, but recent data indicates a worrying shift towards cardiovascular disease as the leading cause of maternal mortality in the United States. With a significant increase in cases of hypertension and other heart-related issues among younger individuals, it is evident that chronic conditions are emerging as critical factors affecting maternal health outcomes. This trend necessitates a reevaluation of maternal care, focusing on preventative measures and the management of pre-existing health conditions that could complicate pregnancy.
The transition in causes of pregnancy-related deaths highlights the need for integrated care models that include screening for chronic health issues prior to and during pregnancy. Understanding this shift can inform healthcare providers and policymakers alike to develop targeted interventions that address cardiovascular health in expecting mothers. By focusing on proactive management of cardiovascular risks and ensuring women have access to appropriate resources and support, we can aim to reverse these dangerous trends and reduce the incidence of maternal mortality.
The Need for Enhanced Data Tracking in Maternal Health
The absence of a consistent and comprehensive system for tracking maternal deaths in the United States has significantly hindered efforts to understand and address the crisis of maternal mortality. Until 2018, the country lacked a national mechanism to accurately capture data on pregnancy-related deaths, making it challenging to identify trends and disparities over time. The introduction of a pregnancy checkbox on death certificates has improved data collection efforts, but continued investment is needed to ensure all states implement this effectively and that the data is utilized to inform health policies and practices.
This lack of comprehensive data can lead to a misunderstanding of the scope of maternal health issues and impede the ability to target interventions effectively. An enhanced maternal health data infrastructure is fundamental to tracking and analyzing pregnancy-related outcomes, ultimately leading to improved care strategies. By prioritizing robust data collection, researchers and policymakers can better understand the intersections of race, ethnicity, and health outcomes, paving the way for informed decision-making that addresses the root causes of disparities in maternal health.
Innovative Solutions for Improving Maternal Health Outcomes
To combat the rising rates of maternal mortality, innovative approaches to healthcare delivery are essential. This includes redefining existing care models to ensure that they are accessible, culturally sensitive, and effective in addressing the specific needs of diverse populations. Creative solutions such as telehealth services, community outreach programs, and mobile health units can help bridge gaps in maternal care, especially in underserved communities. By leveraging technology and community resources, healthcare providers can enhance their reach, ensuring that all pregnant individuals receive the care and support they need during and after pregnancy.
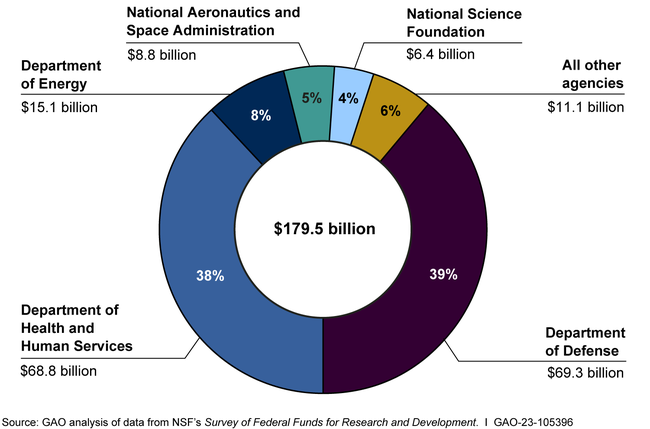
Furthermore, collaboration between healthcare systems, community organizations, and policymakers can foster an environment that prioritizes maternal health. Aligning these stakeholders toward common goals can lead to innovative policy changes that support maternal well-being. Adequate funding and resource allocation for maternal health initiatives are crucial to sustaining efforts aimed at reducing maternal mortality rates. As we invest in new solutions and address systemic barriers, we can foster healthier outcomes for mothers and infants alike.
The Role of Prenatal Care in Maternal Health
Prenatal care is a cornerstone of maternal health that plays an integral role in preventing pregnancy-related deaths. Access to quality prenatal services allows for early identification and management of potential health issues, such as gestational diabetes and hypertensive disorders, which are critical for safeguarding both maternal and fetal well-being. Regular check-ups, screenings, and personalized care enable expected parents to receive guidance and support tailored to their unique circumstances, ultimately laying the groundwork for healthier pregnancies.
Despite the importance of prenatal care, there remain significant barriers that prevent many individuals from accessing these essential services. Structural challenges such as financial constraints, geographic location, and lack of available providers can all contribute to diminished access. To rectify these issues, it is essential to adopt comprehensive policies that ensure equitable access to prenatal care regardless of economic or social factors. By addressing these barriers, we can help create an environment where all pregnant individuals can access timely and effective care throughout their pregnancies.
Policy Changes Needed to Improve Maternal Health
Current state policies exhibit significant disparities in maternal health outcomes, reflecting a patchwork healthcare system that requires urgent reform. The data indicates that if all states performed at parity with California, thousands of pregnancy-related deaths could be avoided. This highlights the critical need for federal and state governments to collaborate on establishing standardized maternal health policies that ensure quality care for all expecting mothers, regardless of their location. Such alignment could lead to equitable healthcare systems that prioritize maternal health as a crucial component of public health.
Substantial investments must be made in maternal health initiatives, focusing on innovation, education, and outreach to vulnerable populations. Policymakers should prioritize research funding, enhance healthcare access, and implement training programs for healthcare providers to deliver high-quality, culturally competent care. By championing these necessary changes, the aim is to create a more responsive healthcare environment that can effectively address and reduce maternal mortality rates while improving overall maternal health outcomes.
Building a Supportive Maternal Health Infrastructure
In order to address the escalating crisis of maternal mortality, it is essential to foster a supportive maternal health infrastructure. This includes not only healthcare facilities but also community resources that contribute to women’s wellness during pregnancy and the postpartum period. By developing comprehensive support networks, we can ensure that expecting mothers have access to vital resources such as mental health services, nutritional counseling, and educational support on pregnancy-related health issues. A robust network can empower women to seek the care they need and promote preventive health measures.
Moreover, investing in public health infrastructure is vital for the development and sustainability of effective maternal health programs. As cuts in healthcare funding threaten existing efforts, it’s imperative to advocate for stronger commitments to maternal health. Addressing the systemic issues that hinder maternal health requires a multifaceted approach, including community engagement, policy advocacy, and increased awareness around the importance of maternal health care. By building a supportive framework, we can work towards drastically improving maternal health outcomes and reducing the risks associated with pregnancy and childbirth.
Frequently Asked Questions
What contributes to the high maternal mortality rates in the U.S. compared to other high-income countries?
The U.S. experiences much higher maternal mortality rates due to its fragmented healthcare system, inequitable health policies, maternity care deserts, and systemic bias, particularly affecting racial and ethnic minorities. Chronic health conditions like hypertension are increasingly common among younger women, further exacerbating risks during pregnancy.
How do health disparities affect maternal mortality rates among different racial groups?
Health disparities significantly impact maternal mortality rates, with studies showing that American Indian and Alaska Native women experience rates nearly four times higher than white women. Non-Hispanic Black women also have elevated mortality rates, highlighting ongoing inequities in maternal health that need addressing through targeted policy changes.
Why are postpartum care and extended health services important in reducing pregnancy-related deaths?
Postpartum care is crucial because nearly a third of maternal deaths occur after the traditional 42-day postpartum window. Recognizing that recovery extends beyond this timeframe emphasizes the need for continuous healthcare support, preventing late maternal deaths and improving overall maternal health outcomes.
What can be done to reduce the rising trends in maternal mortality rates?
To combat rising maternal mortality rates, it’s essential to invest in public health infrastructure and enhance quality care during pregnancy and postpartum. Addressing state-level disparities and promoting innovative healthcare solutions can help improve maternal health outcomes across the U.S.
What role do chronic conditions play in maternal mortality, especially during pregnancy?
Chronic conditions, particularly cardiovascular diseases and hypertension, significantly contribute to maternal mortality rates. These conditions are increasingly prevalent among younger women, and their impact underscores the urgency of integrating better management of chronic health issues into prenatal and postpartum care.
How does the U.S. define pregnancy-related mortality, and why is this definition significant?
In the U.S., pregnancy-related mortality includes deaths during pregnancy and up to one year postpartum. This broader definition is significant as it captures late maternal deaths, highlighting the need for ongoing care beyond the initial postpartum period and informing improvements in maternal health systems.
What are some recommended policy measures to enhance maternal health and reduce pregnancy-related deaths?
Recommended policy measures include increasing healthcare access, improving prenatal and postpartum care quality, investing in maternal health research, and addressing the social determinants of health that contribute to disparities in maternal mortality. Fostering collaboration between states to adopt effective practices can also lead to better outcomes.
| Key Points | Details |
|---|---|
| Maternal Mortality Rate | The U.S. has the highest maternal mortality rate among high-income countries, with 32.6 deaths per 100,000 live births in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are deemed preventable. |
| Disparities | Significant disparities exist based on race and ethnicity, with American Indian women having the highest death rate (106.3), followed by Black women (76.9) compared to white women (27.6). |
| Impact of COVID-19 | The sharpest increase in maternal deaths occurred in 2021, likely due to the COVID-19 pandemic. |
| Racial Inequities | Racial inequities in maternal health persist despite efforts to address them. |
| Postpartum Care | “Late maternal deaths” (deaths from 42 days to a year postpartum) constitute nearly a third of maternal deaths, highlighting the need for long-term maternal care. |
| Need for Policy Change | Investments in public health infrastructure and equitable policies are critical to reduce maternal mortality. |
Summary
Maternal mortality remains a critical public health issue in the United States, with substantial rates that are higher than in any other high-income nation. This tragic reality underscores the urgent need for comprehensive policy reforms aimed at improving maternal healthcare and addressing social disparities. As evidenced by the rising rates of pregnancy-related deaths, particularly among marginalized groups, immediate action is required to ensure that all mothers receive the necessary care throughout pregnancy and afterward. Addressing these systemic issues is essential to making significant progress in reducing maternal mortality and protecting the health of women and children across the nation.